Healthcare disparities expand with reduced subsidy levels
Anúncios
Healthcare disparities expand with reduced subsidy levels, significantly affecting vulnerable populations’ access to essential medical services and leading to worsened health outcomes.
Healthcare disparities expand with reduced subsidy levels, creating significant obstacles for vulnerable populations. How do these changes impact everyday lives and what can be done to bridge the gap? Let’s explore.
Anúncios
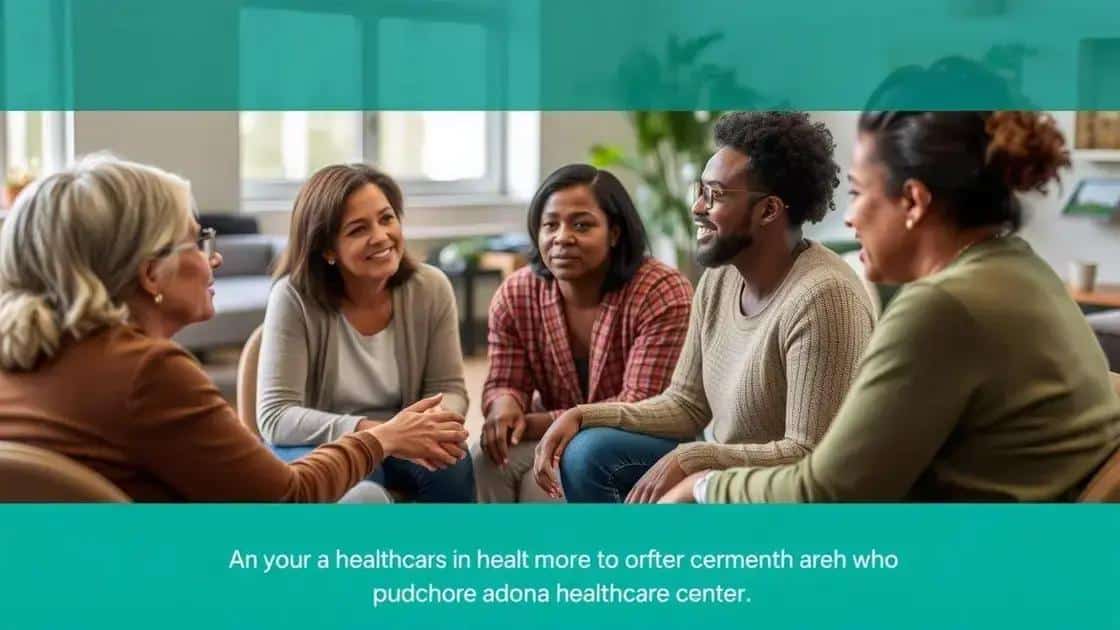
Understanding healthcare disparities
Understanding healthcare disparities is crucial in identifying the inequalities that affect various communities. These disparities can have profound effects on individuals’ health outcomes and overall quality of life.
What Are Healthcare Disparities?
Healthcare disparities refer to the differences in access to or availability of facilities and services. Specific groups may experience barriers to receiving care due to various factors, including socioeconomic status, location, and race. This is not just a statistic; it affects real lives.
Anúncios
Factors Contributing to Disparities
Several elements contribute to the widening gap in healthcare access:
- Economic Barriers: Individuals from low-income backgrounds often face significant obstacles in accessing healthcare services.
- Geographical Location: Rural areas, in particular, may lack the necessary healthcare infrastructure, making it difficult for residents to obtain essential services.
- Education: A lack of health education can lead to misunderstandings of health services and reduced utilization.
- Cultural Differences: Language barriers and cultural misunderstandings can prevent effective communication between patients and healthcare providers.
Understanding these factors is vital as it helps highlight why certain populations are more affected than others. When we look deeper, we begin to see the systemic issues that cause these injustices.
The impact of reduced subsidies is particularly significant. As funding decreases, healthcare providers may be forced to cut services, which disproportionately affects disadvantaged communities. Those in need may find themselves struggling even more as vital resources become limited.
Moreover, the stigma surrounding certain groups can prevent individuals from seeking help. This stigma can stem from cultural beliefs or prior negative experiences within the healthcare system. Addressing these perceptions is a necessary step towards combatting healthcare disparities.
Addressing Healthcare Disparities
Efforts to mitigate these disparities include:
- Policy Changes: Advocating for policies that provide better funding and resources to underserved communities is essential.
- Community Education: Increasing awareness and education about available healthcare services can empower individuals to take charge of their health.
- Building Trust: Healthcare providers need to foster trust within communities by engaging and advocating for the needs of all individuals.
Ultimately, understanding these disparities is the first step in creating a more equitable healthcare system. With concerted efforts, we can work towards a future where everyone has equal access to necessary care, leading to healthier communities overall.
The impact of reduced subsidies on access to care
The impact of reduced subsidies on access to care is significant and far-reaching. As the government cuts back on funding, many healthcare providers struggle to keep their doors open, directly affecting patients in need.
Access Challenges
When subsidies decrease, healthcare facilities may reduce the services they offer, which can lead to longer wait times and increased costs for patients. This is particularly alarming for low-income families who already face numerous barriers to acquiring essential care.
Financial Strain on Communities
Many communities depend on subsidized healthcare to ensure their members can access necessary treatments. With reduced funding:
- Fewer Services: Hospitals and clinics may cut specific programs that are vital for community health.
- Higher Costs: Patients may encounter increased insurance premiums and out-of-pocket expenses as providers adjust to decreased funding.
- Limited Access: Vulnerable populations, such as the elderly and low-income families, often find it even more difficult to seek care.
- Increased Health Disparities: The gap in healthcare equality will widen, impacting those who are already disadvantaged.
The ripple effects of these changes can lead to worsening health outcomes. For example, patients might delay seeking treatment due to increased costs, resulting in more severe health issues over time.
The concern stretches beyond individual patients; entire communities feel the strain when essential health resources are not available. Schools, workplaces, and local economies can all suffer when the population is not healthy.
Long-Term Consequences
As subsidies are cut, we must consider the long-term effects on public health. With fewer resources available, preventative care often takes a back seat, leading to a rise in chronic conditions that could have been managed or prevented with early intervention.
Additionally, healthcare professionals may choose to practice in more affluent areas where funding is stable. This can lead to a shortage of qualified providers in underfunded regions, compounding the difficulties those in less affluent communities face.
In summary, reduced subsidies can create a domino effect that not only limits access to care but also threatens the overall health of communities dependent on these resources.
Communities most affected by disparities

Many communities are significantly affected by healthcare disparities. These disparities stem from various factors, including economic status, geographical location, and social determinants of health. Understanding which communities are most impacted is essential to address these inequalities effectively.
Low-Income Communities
Low-income neighborhoods often face a lack of accessible healthcare services. With fewer clinics and hospitals, residents struggle to receive necessary medical attention. This leads to a cycle of poor health outcomes that can persist across generations. Additionally, financial constraints may prevent individuals from seeking preventive care.
Rural Areas
Rural populations are also deeply affected by healthcare disparities. Geographical isolation means that residents often travel long distances to access care. This can delay treatment for serious conditions. Many rural areas lack specialty services, making it difficult for patients to receive consistent care.
- Transportation Issues: Limited public transport options can make it hard to reach healthcare facilities.
- Provider Shortages: Many rural areas struggle to attract and retain healthcare professionals.
- Emergency Services: Response times for emergencies can be longer in these regions.
The effects on community health are profound, with higher rates of chronic diseases and lower life expectancies reported in many low-income and rural populations.
Minority Communities
Minority groups also experience significant healthcare disparities. These communities may face systemic barriers, including discrimination and cultural misunderstandings. This can result in mistrust towards healthcare providers, making individuals less likely to seek care.
Additionally, linguistic barriers can complicate communication between patients and providers, leading to misunderstandings and inadequate care. The following factors are crucial to consider:
- Cultural Competency: Ensuring that healthcare providers understand diverse cultural backgrounds can improve patient interactions.
- Language Services: Providing translation and interpretation can help in making healthcare accessible.
- Health Education: Targeted health education can empower communities to advocate for their needs.
Addressing the needs of these communities is vital for reducing healthcare disparities. By focusing on outreach, education, and building trust, we can work towards a future where all individuals have equal access to quality healthcare.
Policy changes to address inequities
Policy changes are vital to address inequities in healthcare. Without effective policies, disparities will continue to affect vulnerable populations, preventing them from accessing the care they need.
Importance of Health Policies
Health policies shape the framework within which healthcare services are delivered. They also influence how resources are allocated. By prioritizing fair and equitable policies, we can work towards a more inclusive healthcare system.
Key Policy Changes to Consider
Several crucial changes can help reduce healthcare disparities:
- Funding and Resources: Increasing funding for community health centers can provide essential services to underserved populations.
- Access to Care: Expanding Medicaid in all states would ensure more individuals receive necessary health services without facing financial barriers.
- Preventive Care Programs: Investing in preventive care programs can help identify health issues early, reducing the long-term costs and ensuring better health outcomes.
- Cultural Competency Training: Mandating training for healthcare providers on cultural competency can improve communication and build trust with diverse communities.
Implementing these changes is vital. When policies support better access to healthcare, communities can thrive. Residents are more likely to seek preventive services, leading to healthier populations overall.
Moreover, involving community voices in the policy-making process ensures that the needs of those most affected by disparities are addressed. Policymakers must consult with local leaders and organizations to understand the specific challenges communities face.
Evaluating Policy Impact
After implementing policy changes, evaluating their impact is essential to determine effectiveness. Collecting data on health outcomes, service utilization, and patient satisfaction helps in refining strategies for ongoing improvement. Continuous assessment can lead to better practices that promote equity in healthcare access.
Ultimately, addressing inequities requires a collaborative effort among policymakers, healthcare providers, and communities. By working together, we can create a healthcare system that serves everyone, regardless of their background.
The role of advocacy in healthcare access
The role of advocacy in healthcare access is essential for promoting equity and ensuring that all individuals can obtain the care they need. Advocates work tirelessly to raise awareness about healthcare disparities and push for necessary policy changes.
What Does Advocacy Do?
Advocacy involves various activities aimed at influencing healthcare policies and practices. This can include:
- Raising Awareness: Advocates inform the public and policymakers about healthcare issues affecting specific communities.
- Supporting Legislation: Many advocacy groups campaign for laws that expand access to care, such as Medicaid expansion or increased funding for community health centers.
- Building Coalitions: Collaboration with other organizations strengthens the voice of advocacy efforts, making it more powerful.
- Providing Resources: Advocacy organizations often provide information and tools to help individuals navigate the healthcare system.
By playing these roles, advocates can help to bridge the gap between communities and healthcare providers, ensuring that all voices are heard.
Impact of Advocacy
Advocacy efforts can lead to significant changes in healthcare access. For instance, when communities organize to demand better services, they often see positive outcomes. This might include:
- Increased Funding: Elected officials may allocate more resources to underserved areas.
- Policy Revisions: Laws may be updated to remove barriers that prevent individuals from receiving care.
- Enhanced Community Programs: Funding can lead to the development of programs that directly address local health needs.
These changes are vital for communities facing healthcare inequities. Furthermore, as more individuals become involved in advocacy, a sense of empowerment grows, fostering a culture where community health matters.
Advocacy can also take the form of personal stories. Sharing individual experiences with healthcare inequities can evoke empathy and motivate others to take action. Personal stories remind us that behind the statistics are real people facing real challenges.
Getting Involved in Advocacy
Individuals can engage in advocacy through various means. Volunteering with local organizations, participating in awareness campaigns, and contacting elected representatives are all effective ways to make a difference. Everyone has a voice that can contribute to the movement for better healthcare access.
As communities grow stronger through advocacy, the push for health equity becomes more impactful. Together, collective efforts can lead to lasting change, making healthcare accessible for everyone.
In conclusion, addressing healthcare disparities is crucial for creating a fair system where everyone has access to essential services. Advocacy plays a significant role in pushing for necessary policy changes and ensuring that the voices of affected communities are heard. By working together, we can tackle the barriers that prevent individuals from receiving care. Each of us can contribute to this effort, supporting initiatives that promote equity in healthcare. Together, we can build a healthier future for all.
FAQ – Frequently Asked Questions about Healthcare Disparities and Advocacy
What are healthcare disparities?
Healthcare disparities refer to differences in access to or availability of healthcare services among different populations, often based on factors such as socioeconomic status, race, or geographic location.
How can advocacy help improve healthcare access?
Advocacy raises awareness of healthcare issues and influences policy changes that can expand access to care, ensuring that marginalized communities receive the support they need.
What role do community voices play in advocacy?
Community voices are crucial in advocacy as they provide insight into the specific challenges faced by populations, helping to shape effective policies and programs that address their needs.
Why is it important to track healthcare data?
Tracking healthcare data is essential to evaluate the effectiveness of policies, identify ongoing disparities, and make informed decisions for future improvements in healthcare access.